

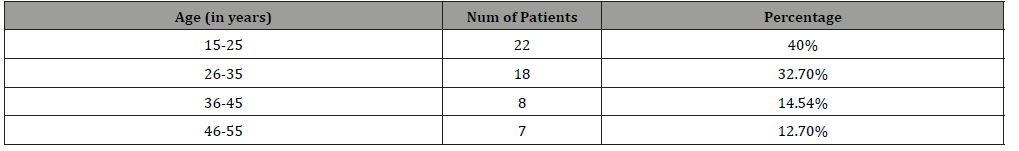
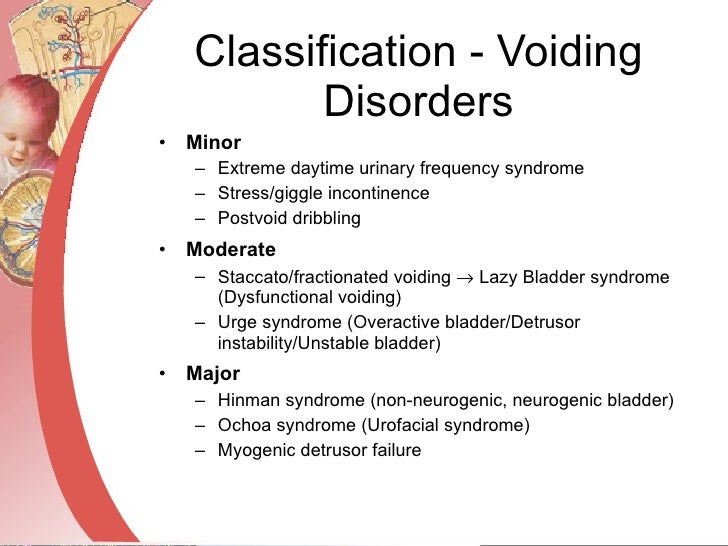
Keywords included ‘male stress urinary incontinence’, ‘overactive bladder’ and ‘urge incontinence’. Methods and evidence synthesisĪ literature search was performed on the PubMed database for English-language, original and review articles published up to December 2016. All treatment options should be discussed to facilitate informed decision-making, and these options can then be individualised on the basis of patient preference, current comorbidities and specific circumstances. 1,3 This article briefly reviews the current understandings of the pathophysiological mechanisms in SUI and OAB/UUI, and offers a set of practical, action-based recommendations and treatment strategies. Persistent, non-neurogenic urinary incontinence in adult males can be classified as stress urinary incontinence (SUI), OAB with urge urinary incontinence (UUI), mixed incontinence, overflow (paradoxical) incontinence, continuous urinary incontinence (eg fistula) and functional incontinence. 1 The presence of poor general health, medical comorbidities, severe physical limitations, cognitive impairment, neurological conditions, recurrent urinary tract infection (UTI) and prostatic diseases have been associated with urinary incontinence. 2 The prevalence of urinary incontinence increases with age and it is estimated that more than one in four men aged over 70 years have urinary incontinence. 1 A Deloitte Access Economics report commissioned by the Continence Foundation of Australia found that more than 4.2 million Australians aged 15 years and older had urinary incontinence in 2010. Lower urinary tract dysfunction, such as benign prostatic hyperplasia (BPH), overactive bladder (OAB) and urinary incontinence, are common conditions that adversely affect health-related quality of life and increase the risk of institutionalisation.


 0 kommentar(er)
0 kommentar(er)
